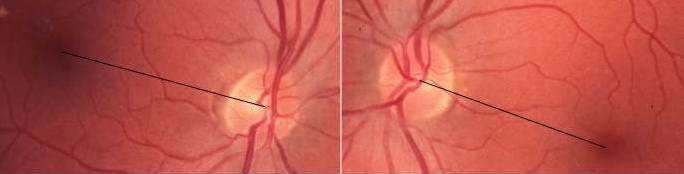
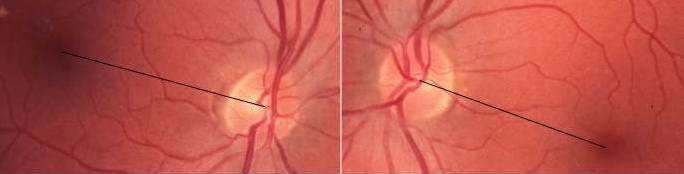
Among all the neuro-ophthalmological manifestations of brainstem disease, bilateral torsion of the eyes is the most timid one. Although torsions may reach remarkable degrees, even 30° and more, they do not advertise themselves, neither to the affected subject, nor to the examiner. Subjective recognition requires removal of visual references to true vertical and horizontal, for example, by looking into a suitably prepared wastepaper basket, and objective recognition requires a goal-directed examination of fundus landmarks. The use of either technique (or both) will be richly rewarded because asymptomatic torsion of the eyes is very common indeed, with a reported prevalence of 94% among patients with acute lesions of the brainstem [1]. The montage below shows an example of acquired ocular torsion due to a lateral medulla infarct, with about 15° of clockwise conjugate torsion. There was no subjective corollary.
Asymptomatic ocular torsion, abbreviated AOT in the following, is sometimes combined with skew deviation and head tilting and then forms part of the ocular tilt reaction, OTR, but isolated AOT is much more common than the full OTR syndrome. The high prevalence indicates that the neural substrate is widely spread over the brainstem. In brief, it is thought to involve pathways that carry vestibular signals via the vestibular nuclei and vertical ocular motor control structures in the upper midbrain to the oculo-rotatory muscles [2].
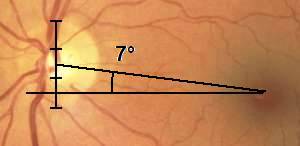 How do acquired bilateral torsions escape detection? The major reasons are the paucity of anatomical landmarks plus normal variation. An old rule-of-thumb says that a transversal line through the fovea will intersect the disc at about two-thirds of the disc height. However, there is considerable variation. Quantitative measurements show that a line connecting the fovea and the disc center forms an angle relative to the transversal line of about 6°, on average. Normal limits range over some 0 to 12°
[3].
Hence, it is quite easy to overlook torsion. At the bedside, the best approach may be to apply the rule-of-thumb construction and compare the two eyes: normally, the heights of intersection should be closely similar.
How do acquired bilateral torsions escape detection? The major reasons are the paucity of anatomical landmarks plus normal variation. An old rule-of-thumb says that a transversal line through the fovea will intersect the disc at about two-thirds of the disc height. However, there is considerable variation. Quantitative measurements show that a line connecting the fovea and the disc center forms an angle relative to the transversal line of about 6°, on average. Normal limits range over some 0 to 12°
[3].
Hence, it is quite easy to overlook torsion. At the bedside, the best approach may be to apply the rule-of-thumb construction and compare the two eyes: normally, the heights of intersection should be closely similar.
Subjective corollaries of torsion are lacking in AOT, by definition. From the subject's point of view, there is nothing wrong. When asking the subject to orient a test object to a vertical position, he or she will do so correctly. However, on removal of external references to true vertical, the subject will re-orient the object to match the torsion of the eyes. He or she will not see the error until the external references are shown again. This behavior suggests the operation of central mechanisms that draw on life-long experience with external references to rectify absurd tilts.
 The diagram shows the relationship between objective torsions and subjective deviations in a group of 38 subjects with a variety of acute brainstem lesions. Torsions were measured in pairs of fundus photographs and subjective devations were assessed binocularly with the
wastepaper basket
test. The variation about the regression line derives from multiple factors, including different geometries of the non-simultaneous measurements. Notably, subjective measurements have narrower normal limits (about ± 2°) than objective measurements, indicating that subjective tests have the better potential to identify low-degree abnormalities.
The diagram shows the relationship between objective torsions and subjective deviations in a group of 38 subjects with a variety of acute brainstem lesions. Torsions were measured in pairs of fundus photographs and subjective devations were assessed binocularly with the
wastepaper basket
test. The variation about the regression line derives from multiple factors, including different geometries of the non-simultaneous measurements. Notably, subjective measurements have narrower normal limits (about ± 2°) than objective measurements, indicating that subjective tests have the better potential to identify low-degree abnormalities.
It is interesting to ponder why subjects with AOT and subjects with peripheral nerve lesions differ in their perceptions of ocular torsion. Subjective recognition of torsion is certainly common with peripheral lesions, not the least 4th nerve palsies. The explanation presumably relates to torsional symmetry and fusion: symmetrical torsion allows fusion, but asymmetrical torsion does not. This can be observed with the aid of two Maddox rod lenses. When viewing a
 point source of light through a Maddox rod lens, the light source will be seen as a bright line centered on the line of sight. On rotation of the lens, the line
will also rotate. Using one lens in front of each eye, with the grooves oriented horizontally to generate vertical lines, non-strabismic subjects can easily fuse each eye's line to a single line. Conjugate rotations of the lenses will not interfere with fusion, but rotation of one lens only will cause fusion to break.
point source of light through a Maddox rod lens, the light source will be seen as a bright line centered on the line of sight. On rotation of the lens, the line
will also rotate. Using one lens in front of each eye, with the grooves oriented horizontally to generate vertical lines, non-strabismic subjects can easily fuse each eye's line to a single line. Conjugate rotations of the lenses will not interfere with fusion, but rotation of one lens only will cause fusion to break.
Another difference between AOT and paretic eyes is that the latter usually also suffer from tropic deviations (eso/exo, hyper/hypo), which by themselves frequently hinder fusion.
 The wastepaper basket and related laboratory tests assess the subjective deviations associated with ocular torsions in the fronto-parallel or roll plane. Monocular and binocular roll tests usually return similar but rarely identical results, suggesting that binocular fusion of the monocular images should result in a subjective deviation also in depth, in the sagittal or pitch direction. Consider the projection of imaginary retinal vertical meridians into external space, on to a convergence point. Normally, the planes' intersection defines a vertical line, through the convergence point. Conjugate torsions of the eyes will cause the line of intersection to deviate in roll whereas disjugate torsions will cause a deviation in pitch. These effects can be illustrated in animated displays; these have been placed on a
separate page to minimize eye fatigue.
The wastepaper basket and related laboratory tests assess the subjective deviations associated with ocular torsions in the fronto-parallel or roll plane. Monocular and binocular roll tests usually return similar but rarely identical results, suggesting that binocular fusion of the monocular images should result in a subjective deviation also in depth, in the sagittal or pitch direction. Consider the projection of imaginary retinal vertical meridians into external space, on to a convergence point. Normally, the planes' intersection defines a vertical line, through the convergence point. Conjugate torsions of the eyes will cause the line of intersection to deviate in roll whereas disjugate torsions will cause a deviation in pitch. These effects can be illustrated in animated displays; these have been placed on a
separate page to minimize eye fatigue.
More direct ways to visualize how disjugate image torsions will generate sensations of depth includes looking through two Maddox rod lenses or two Dove prisms. The suggestion to use dual Maddoxes may be surprising as it was stated above that disjugate rotations will interfere with fusion. The statement remains true for casual observers but a closer look reveals that loss of fusion applies primarily to the outer parts of the images: attention to the central parts allows fusion and generates a sensation of depth. In case of difficulty, it helps to decrease the lens apertures, e g, by means of adhesive tape.
In contrast to Maddox rod lenses, Dove prisms provide natural images of the external world. These prisms have the unusual property of turning the field of view around the line of sight on rotation of the prisms around their long axes. Because Dove prisms also flip the field of view laterally, two prisms are needed, one in front of each eye. It is also possible to use plain right-angle prisms and direct the lines of sight parallel to their hypotenuses, but plain prisms produce smaller fields of view. It is best to view a vertical line drawn on a uniform background. Again, conjugate rotations will generate deviations in roll and disjugate rotations will generate deviations in pitch.
 Neither the wastepaper basket nor related laboratory tests can assess subjective deviations in depth. This requires a
different set-up,
where the test task is not constrained to adjustment in roll, but also allows adjustment in pitch.
Neither the wastepaper basket nor related laboratory tests can assess subjective deviations in depth. This requires a
different set-up,
where the test task is not constrained to adjustment in roll, but also allows adjustment in pitch.
In a recent study of 40 subjects with various focal brainstem lesions, the combined test uncovered deviations in roll only in 10%, in pitch only in 38%, and in roll plus pitch in 28%. Hence, deviations were more common in pitch than in roll. Further, deviations were generally larger in pitch than in roll. Overall, there was no correlation between pitch and roll results, and none was expected. On the other hand, differences in roll between the two eyes should correlate with deviations in pitch. See [4] for a full report.
The graviceptive system is very complex and includes both vestibular and somatosensory components and a multiplicity of connections, commissures, pathways, and targets. Its functions have been explored in many ways and in great detail, not the least with regard to the semicircular canals and their influence on eye movements. The canals signal endolymph movement by modulating their rate of firing, increasing the rate with movement in one direction and decreasing the rate in the other. The rate of firing is intermediate at rest, suggesting that the canals contribute to the resting tone of the extra-ocular eye muscles. The otolith systems appear to use similar signal modulations and projections [5].
For a first orientation, it is practical to focus on a single semicircular canal and its projections to the extra-ocular muscles. This is not meant to imply that AOT generally is attributable to a primary involvement of a single canal or otolith subsystem. Actually, movement-related signal modulations are not germane to AOT because AOT is present at rest. Instead, it is proposed that the AOT associated with brainstem lesions is attributable to a an impaired up-stream transmission of normally generated resting signals.
 The diagram to the right aims to reduce the complexity of the vestibulo-ocular system to a bare minimum, by focusing solely on the relations between the right anterior semicircular canal and the right and left oculo-rotatory muscles (R is brief for rectus, O for oblique, S for superior, and I for inferior; the arrows indicate main directions of action).
The anterior canal normally provides a resting tone to the ipsilateral RS and the contralateral OI muscles. A decreased resting tone (red arrows) results in antagonist dominance (green arrows), causing a depression plus some extorsion on the right and an intorsion plus some depression on the left. A similar reasoning can be applied to the posterior semicircular canal (which provides a resting tone to the ipsilateral OS and contralateral RI) and to both canals in combination and in varying proportions. It is likely that a similar reasoning may be applied to the otolith projections. (The lateral semicircular canal projects to the lateral and medial rectus muscles, which are not involved in torsion (but possibly in lateropulsion of the eyes, which sign sometimes accompanies AOT)).
The diagram to the right aims to reduce the complexity of the vestibulo-ocular system to a bare minimum, by focusing solely on the relations between the right anterior semicircular canal and the right and left oculo-rotatory muscles (R is brief for rectus, O for oblique, S for superior, and I for inferior; the arrows indicate main directions of action).
The anterior canal normally provides a resting tone to the ipsilateral RS and the contralateral OI muscles. A decreased resting tone (red arrows) results in antagonist dominance (green arrows), causing a depression plus some extorsion on the right and an intorsion plus some depression on the left. A similar reasoning can be applied to the posterior semicircular canal (which provides a resting tone to the ipsilateral OS and contralateral RI) and to both canals in combination and in varying proportions. It is likely that a similar reasoning may be applied to the otolith projections. (The lateral semicircular canal projects to the lateral and medial rectus muscles, which are not involved in torsion (but possibly in lateropulsion of the eyes, which sign sometimes accompanies AOT)).
The above model predicts a combination of torsional and vertical devations but the latter are typically lacking in AOT. A likely explanations is that eye positions are governed not only by vestibular tone but also by supranuclear eye movement controls. These are primarily geared for horizontal and vertical eye movements and may be able to override vertical deviations but not torsions. In the presence of a vertical deviation, skew devation is a more appropriate description, and if combined also with a head tilt, the proper designation is an ocular tilt reaction, OTR.
Considering the complexity and the wide distribution of the neural substrates for deviations in pitch and roll as well as the size of clinically manifest lesions, deviations in pitch and/or roll are likely to have a limited value for topograhic diagnosis, even if the directions of the deviations are taken into account. As to roll, clockwise deviations (as seen from the subject's side) are suggestive of right-sided lesions and vice versa whereas backward deviations in pitch (top toward the subject) are suggestive of dorsal midbrain lesions. However, there are many exceptions. Further, deviations may arise with both focal and non-focal lesions. Deviations in pitch are particularly common with obstructive hydrocephalus.
The major role of testing for subjective deviations is not to aid topographic diagnosis but to help rule in or rule out the presence of structural lesions in subjects who have histories suggestive of brainstem disease but lack overt clinical signs. Further, in subjects who do return abnormal results, repeated testing helps to monitor the evolution of the underlying disorder. In subjects who do improve, deviations may disappear within a few days or weeks.
 Although the test tools described above are fairly simple, there is a still simpler approch that requires neither fabrication, nor darkroom facilities. Actually, two Maddox rod lenses should do equally well. For best results, the lens apertures should be reduced to some 8 millimeters diameter, using sticky tape or plain discs cut from a piece of cardboard, and the lenses should be placed in a carefully positioned trial lens frame. A distant point source of light is also needed - a single LED-type flashlight is ideal. It may be useful to reduce room illumination to obtain a high contrast.
Although the test tools described above are fairly simple, there is a still simpler approch that requires neither fabrication, nor darkroom facilities. Actually, two Maddox rod lenses should do equally well. For best results, the lens apertures should be reduced to some 8 millimeters diameter, using sticky tape or plain discs cut from a piece of cardboard, and the lenses should be placed in a carefully positioned trial lens frame. A distant point source of light is also needed - a single LED-type flashlight is ideal. It may be useful to reduce room illumination to obtain a high contrast.
Make sure the subject is seated comfortably, in the upright position. Cover one eye and ask the subject to rotate the lens in front of the viewing eye so as to make the luminous line perfectly vertical. If the subject finds the manual adjustment difficult, the examiner can take over, guided by the subject's responses. When done, read the roll angle from the trial frame's protractor scale and repeat the procedure for the second eye. This is all that is needed to assess monocular deviations in roll.
To extend the examination for deviations in pitch, proceed as follows. Remove the eye cover and allow the subject to fine-tune the rotation of either lens to obtain comfortable binocular viewing. Now ask the subject if the top of the luminous line appears to tilt towards or away from the subject. If a tilt is perceived, an index of its magnitude can be obtained by asking the subject to rotate one or the other lens until the line appears to be perfectly vertical in depth.
Note that the trial frame must be aligned very carefully to allow meaningful use of the protractor scales. Further, angles need to be read to the nearest degree, particularly when attempting to assess deviations in depth.
 Another way to assess the subjective visual vertical in roll and pitch is to use an adjustable anaglyphic display like the figure to the right, viewed through red and and cyan (or green) filters for the left and right eyes, respectively. On rotation of the two bars around their centers in a conjugated fashion, the fused image will appear to rotate in the frontal plane, that is, in roll. On rotation of the two bars around their centers in a disjugated fashion, the fused image will appear to rotate in the sagittal plane, that is, in pitch. The test task is to adjust the perceived bar orientation to perfect verticality, in both roll and pitch. The two circles are stationary and serve as a fixed reference to depth in space.
Another way to assess the subjective visual vertical in roll and pitch is to use an adjustable anaglyphic display like the figure to the right, viewed through red and and cyan (or green) filters for the left and right eyes, respectively. On rotation of the two bars around their centers in a conjugated fashion, the fused image will appear to rotate in the frontal plane, that is, in roll. On rotation of the two bars around their centers in a disjugated fashion, the fused image will appear to rotate in the sagittal plane, that is, in pitch. The test task is to adjust the perceived bar orientation to perfect verticality, in both roll and pitch. The two circles are stationary and serve as a fixed reference to depth in space.
Click on the image to open the anaglyphic display in a separate window. Use horizontal mouse movements to produce conjugate rotation of the bars. Use vertical mouse movements to produce disjugate rotation. The current angles of rotation are indicated in the upper left corner of the display. The numbers are shown at low contrast to provide minimum distraction. The indicated roll angles are true; the pitch angles are nominal.
Note that any external references to true vertical and horizontal orientations, for example, the display's edges, will prevent subjective perception of any ocular torsions. Therefore, the test area must be viewed through a screening tube that excludes all outside references. Such a tube can easily be rolled from a piece of corrugated cardboard. The tube's length should equal the viewing distance, similar to the 2D wastepaper basket test mentioned above.